Abstract
INTRODUCTION: Since the onset of the COVID-19 pandemic, clinicians and researchers have sought to understand who is at risk of severe disease. Although children are more likely to have mild disease than adults, children with underlying health conditions (including cancer and Down syndrome [DS]) are at increased risk for severe infection. Children with cancer and COVID-19 have higher rates of hospitalization, ICU admission, and death when compared with children without cancer; they are also at risk of having their cancer therapy modified [Johnston...Wolfson; JCO 2021]. Children with DS and hematologic malignancies are a particularly vulnerable group in terms of cancer-related toxicities (infection-related mortality in particular). This has led to changes in treatment and supportive care protocols to decrease infection-related mortality for children with DS and hematologic malignancies. However, there are limited data regarding COVID-19 infections in this vulnerable group. We leveraged the Pediatric Oncology COVID-19 Case (POCC) Report registry to understand the clinical course of COVID-19 infection and optimize care in children with hematologic malignancies and DS.
METHODS: POCC captures de-identified data from >100 sites (>50% of US pediatric oncology sites). Sites submit data regarding patients with a malignancy at age <40y and COVID-19 during cancer therapy or within 12 months of completing therapy. Sites submit sociodemographics, clinical and treatment details, known comorbidities, and the clinical course of COVID-19 within 12 weeks of infection (symptoms, support needed for COVID-19 infection and changes in cancer therapy).
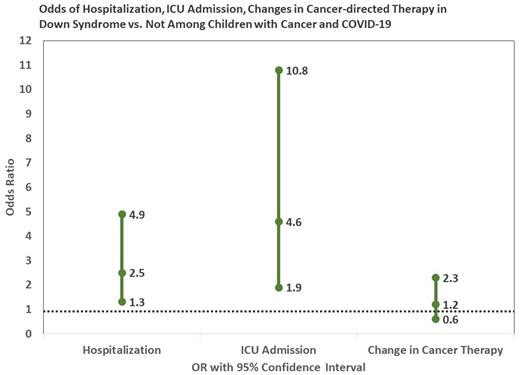
We constructed a cohort of children (≤21y at COVID-19 infection) with hematologic malignancies reported to POCC between 4/1/20 and 5/18/22. Primary outcomes of interest were hospitalization, ICU admission, and changes in cancer therapy. Multivariable logistic regression compared the odds of hospitalization, ICU admission, and changes in cancer therapy among DS and non-DS patients (adjusting for age at COVID-19 infection, sex, race/ethnicity, payor, cancer diagnosis, relapse status, blood or marrow transplant [BMT] status, absolute neutrophil count [ANC] at infection and comorbidities).
RESULTS: Among 1,157 children with hematologic malignancies and COVID-19, 47 (4%) carried a DS diagnosis; 12-week follow-up data were complete in 98%. The median age at infection was similar in children with (10y, IQR: 5-16) and without (9y, IQR: 4-14.0; p=0.98) DS. Most children were publicly insured (DS=60%, non-DS=58%, p=0.98), while those with DS were more often Hispanic (DS=64%, non-DS=41%; p=0.03). The most common diagnosis was acute lymphoblastic leukemia ([ALL]: DS=94%, non-DS=74%; p=0.02). Few children had relapsed disease (DS=13%, non-DS=14%, p=0.78) or a history of BMT (DS=2%, non-DS=9%; p=0.18). Additional comorbidities were reported in 34% of DS and 22% of non-DS children (p=0.06). More children with DS (DS=13%, non-DS=10%; p=0.02) had an ANC <500 at the time of infection. No patients with DS died due to COVID-19.
Hospitalization and ICU admissions: Children with DS were more likely to be hospitalized (DS=57%, non-DS=30%, p<0.01; OR=2.5, 95%CI 1.3-4.9) and admitted to the ICU (DS=19%, non-DS=7%, p<0.01; OR=4.6, 95%CI 1.9-10.8). Children with DS also more often required either respiratory (DS=28%, non-DS=8%; p<0.01 [supplemental oxygen: 13% vs. 6%; mechanical ventilation: 11% vs. 2%; BiPAP: 4% vs. 1%]) or other (DS=6%, non-DS=2%; p<0.01 [vasopressors, ECMO, dialysis]) support. [Fig1]Therapeutic Modifications: While half of DS patients (49%) had their cancer-directed therapy changed, there was no statistically significant difference between DS and non-DS patients (OR=1.2, 95%CI 0.6-2.3).
DISCUSSION: Children with DS are a particularly vulnerable sub-population of children who face even greater risks than other children with hematologic malignancies when they develop COVID-19. These data can inform conversations with patients and families regarding the use of preventive measures that are pharmacologic (vaccines and pre/post-exposure prophylaxis) and non-pharmacologic (masking) as well as the risks and benefits of modifying chemotherapy and other therapeutic measures for patients who become infected (antivirals, monoclonal antibodies).
Disclosures
Dickens:Tempus: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal